Ambulance Patient Offload Time and Transfer of Care Information

EMS Authority APOT Mandate
Ambulance Patient Offload Time (APOT) is the time from ambulance arrival at a receiving facility until the formal transfer of care is completed.
-
Why it matters:
- Ambulance unit turnover of care delay
- Reduced EMS system availability
- Continuity of care
-
Regulatory requirements:
- California AB 40 (2023) mandates the EMS Authority to adopt a standardized APOT audit framework.
- EMSA has published emergency regulations (Regulation Text) to implement AB 40.
- EMSA’s APOT program (emsa.ca.gov/apot) is the hub of technical specs, audit tools, reporting, and outreach.
- The San Diego County EMS APOT time standard is 30 minutes (County EMS Policy S-610).

APOT Time Interval
The Ambulance Patient Offload Time (APOT) represents the total elapsed time between when an ambulance arrives at a hospital emergency department and when patient care is formally received by hospital staff. This metric is standardized statewide to measure emergency department offload efficiency.

Start of Measurement — Arrival at Destination Facility
- Event: The ambulance arrives at the hospital to begin patient offload.
- NEMSIS Field: eTimes.11 – Patient Arrived at Destination Date/Time
- Description: Timestamp when the ambulance reaches the emergency department and the patient is available for hospital evaluation (e.g., wheels stop at ED ambulance bay or crew enters receiving facility/care area).
- Method: This datapoint may be established by ePCR button push or via a Computer-Aided Dispatch (CAD ) integration. CADs may record the ambulance arrival at an ED through GPS-triggered processes.
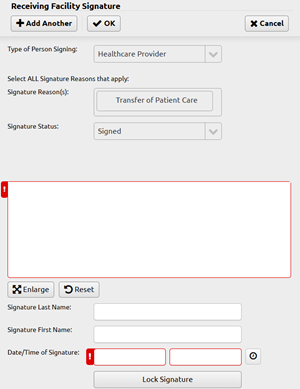
Receiving Facility Signature Time
-
Event: The standardized transfer of patient care is completed
when:
- The patient is physically transferred to a receiving facility gurney, bed, chair, or other mutually agreed upon and safe location
- AND EMS personnel provide a patient-centered verbal patient report to the receiving facility medical personnel
- AND Receiving facility medical personnel sign the ePCR and assume patient care
- NEMSIS Field: eOther.19 – The date/time the Signature of Person Receiving Patient Care signature was captured
- Description: When an ambulance patient is physically transferred to an emergency department gurney, bed, chair, or other acceptable location, and emergency department medical personnel receives the report and confirms the transfer of patient care with an electronic signature within the ePCR
-
Relationship to eTimes.12:
- The signature time typically corresponds to the eTimes.12 timestamp and may be used to validate the overall Transfer of Care interval.
- For compliance and auditing purposes, eTimes.12 should reflect the time the receiving signature timestamp recorded in the ePCR or LEMSIS.
- Discrepancies between eTimes.12 and the signature time should be minimal.
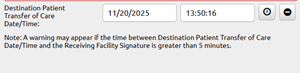
End of Measurement — Transfer of Care
- Event: The receiving hospital staff has received the formal transfer of patient care.
- NEMSIS Field: eTimes.12 – Destination Patient Transfer of Care Date/Time
- Description: Timestamp representing the moment of official patient handoff to hospital personnel. This marks the end of the offload interval.
- Method: This data is recorded in the ePCR through a date/time field. In the LEMSIS PCR, the field is named Destination Patient Transfer of Care Date/Time. This field appears directly below the Receiving Facility Signature data group.

Under AB 40 and the related regulations, each civilian General Acute Care Hospital (GACH) with an emergency department can validate and reconcile APOT data using a statewide electronic Audit Tool. The aim is to ensure accuracy in measuring transfer-of-care times (NEMSIS eTimes.11 → eTimes.12) and to identify system or workflow barriers that cause delays in offloads.
Data Submission and Audit Timeframes
Monthly Submission:
- EMS transport providers submit APOT data through the California EMS Information System (CEMSIS) automatically via LEMSIS.
- EMS transport providers not in compliance with Health and Safety Code Section 1797.223 are excluded from the APOT data.
Hospital Audit Process and Timeframe:
- Hospital administrators review APOT data provided by the EMSA Audit Tool and identify any discrepancies, including those between electronic health record (EHR) or other administrative tracking system timestamps and CEMSIS-reported times.
- The APOT Audit Tool aims to improve the accuracy and confidence in EMS APOT data for EMS providers, LEMSAs, and hospitals.
- EMSA recommends that hospital staff focus on APOT records that are most likely to impact the facility's APOT compliance metric, rather than reviewing all records.
Discrepancy Notification:
- Once hospital administrators submit any discrepancies through the monthly APOT Audit Tool, automated email notifications are sent to County EMS and the involved EMS provider(s) regarding any data mismatches.
- EMS Agencies will receive a list of flagged PCR numbers by email. LEMSIS users may wish to use the LEMSIS EMS Incident System View PCR # Audit Tool to find the PCRs included in this notification.
- EMS Agencies with records included in an audit, beginning October 14, 2025, may receive Audit Tool comments and other information through these automated notifications.
State EMSA APOT Compliance Meetings
- EMSA may convene bi-weekly coordination calls whenever APOT standards are exceeded;
- These meetings will continue until hospitals demonstrate sustained compliance with the adopted local APOT standard for two consecutive reporting periods.
Data Elements and Compliance Validation
911 ambulance transports to in-county civilian hospital emergency departments are included in the EMSA APOT compliance metrics. Interfacility, nonemergency, or ground ambulance transports to emergency departments outside San Diego County are excluded from EMSA APOT evaluation.
The APOT Audit Tool verifies consistency among the following NEMSIS 3.5 elements (from the Technical Specifications and Clarification of APOT-1 Technical Specifications memo):
- eTimes.11 – Patient Arrived at Destination Date/Time
- eTimes.12 – Destination Patient Transfer of Care Date/Time
- eOther.12 – Type of Person Signing (Healthcare Provider)
- eOther.13 – Signature Reason (Transfer of Care)
- eOther.19 – Date/Time of Signature
Records must be logical, complete, and signed; any negative or illogical intervals are excluded.
County EMS Office Role
- Collects and reviews monthly CEMSIS data
- Coordinates audit discrepancy meetings with hospitals and agencies.
- Ensures corrections are submitted by the 15th of each month.
- Reports audit results and patterns to EMSA and local stakeholders.
- Facilitates ongoing quality improvement efforts.